Written by a CuraCore Veterinary Medical Acupuncture course graduate. Signed release obtained from client/author. 10S2019002
Abstract
Francis, a two-year-old intact male English Bulldog, presented for an acupuncture consultation to address mobility issues stemming from a number of congenital abnormalities. The goals for the owner were to increase and then maintain mobility, decrease any pain, and to try to wean his medication (steroid). He was treated once weekly with acupuncture and massage. He was treated for four weeks with plans to continue as the owner reported a favorable response in his mobility after only a few sessions.
Francis before rehab consult May 2018
History and Presentation
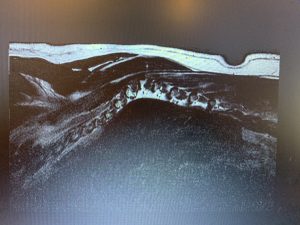
Francis is a two year old, intact male, English Bulldog who was rescued from a puppy mill/hoarding situation at approximately eight weeks of age. The owner (foster mom) initially noted mild, bilateral, carpus valgus that progressed over the next month. The left carpus was more severely affected. Over the next two months (age 4-6 months) Francis developed progressive paraparesis and ataxia in the pelvic limbs. He was seen for an initial neurology consult on Jan 16, 2018 (six months of age). His exam at that time revealed normal cranial nerves, carpal valgus (more severe on the left), normal neurologic exam in the thoracic limbs, moderate to severe upper motor neuron (UMN) paraparesis and ataxia in the pelvic limbs. He had absent postural reactions bilaterally, hyper tone and reflexes. He had normal femoral pulses, anal tone, and perineal reflexes. He did not appear to have spinal pain. A T3-L3 myelopathy associated with vertebral malformations was suspected. The rescue elected to have additional diagnostics performed in order to obtain a definitive diagnosis. Additional diagnostics included a complete blood count and chemistry panel, spinal radiographs, and MRI. Blood tests were within normal limits. Spinal radiographs (cervical, thoracic, and lumbar) revealed numerous malformed vertebrae and an abnormal curvature of the spinal column. MRI revealed severe scoliosis and kyphosis associated with vertebral malformations from T5-T10 causing moderate to severe left sided spinal cord compression. Medical management was elected to alleviate some of the paresis and ataxia associated with the spinal cord compression. Francis was started on dexamethasone (0.5 mg every twelve hours) until his next appointment. A controlled regime of activity was recommended and the owners were instructed to avoid high impact activities such as running, jumping, and rough play. The owners were also instructed to avoid slippery surfaces and to use a harness to help support his rear end during walks.
At his initial recheck appointment (1/20/2018), Francis had mild improvement. He was falling less and getting around better. He had decreased postural reactions (left greater than right), hyper tone and reflexes. He was having severe polyuria and polydipsia (PU/PD) from the steroid. The owner and neurologist did not feel that Francis was painful. His steroid dose was decreased from twice a day to once a day. He was sent home with the same instructions as far as activity as he was initially.
At the second recheck appointment (2/13/2018), Francis had declined slightly. The owner felt he was more wobbly and falling more. His exam was unchanged and his steroid dose was increased to 0.5 mg in the am and 0.25 mg in the pm.
Francis had two additional rechecks with the neurologist (4/17/2018 and 8/9/2018) and his clinical signs were static. He was still ataxic in the pelvic limbs, however, he was able to get up and walk a short distance before falling. The owner had decreased his steroid dose to 0.5 mg once a day on her own during this time. He was found to be moderately ambulatory with moderate UMN paraparesis and ataxia, decreased postural reactions, hyper tone and reflexes, and no spinal pain. The owner was instructed to continue the same steroid dose (0.5mg once a day) and continue with the same regime for activity. Recommendations were made to purchase a cart for long term management as well as keeping the dog thin.
The owner did not recheck after the last appointment on 4/17/2018. He worsened over the next month and the owner elected to consult with a rehabilitation veterinarian. His initial consult was on May, 23, 2018. Francis was unable to walk on his own (pelvic limbs) and would drag himself on his stifles. Motor was present in both pelvic limbs; he had slow withdrawal reflexes bilaterally, and did not appear painful. He had severe carpal valgus on the left. He was able to stand when placed and with intermittent support. His body condition was rated as a 5/9.
Recommendations were made for in-clinic rehabilitation twice weekly focusing on pelvic limb strengthening and neurological re-education. The owner was also given home exercises to do. Home exercises included assisted standing with weight shifting, assisted sit to stands, assisted transitions from lateral laying to sternal laying, strike a match, toe tickles, knuckle exercises, and passive range of motion exercises. The owner did home exercises in short intervals as to give Francis time to rest. Because of his breed related upper airway issues, it was important to make sure he did not exert himself to the point of respiratory distress. While the owner continued to do home exercises on her own, financial decisions by the rescue made in-clinic rehabilitation impossible.
Francis 1st eval Nov 6, 2019-neck tightness and rear limb weakness
Physical Exam and Clinical Assessment
On presentation Francis was bright, alert, and responsive. He was happy, friendly and interactive. His vital signs were all within normal limits. He was taking dexamethasone 0.25 mg every other day and Dasuquin once daily. He had a body condition score of 5/9. He had upper airway stertor common for a brachycephalic breed. This stertor worsened with excitement and when we attempted to have him lay on his side. He had bilateral carpal valgus that was more severe on the left. He was ambulatory on all four limbs with mild pelvic limb ataxia. His cranial nerves were normal. Forelimb neurologic exam appeared normal but was limited due to his reluctance to lie still or on his side before becoming stressed. He had normal conscious proprioception (CP) and withdrawal in the thoracic limbs. He had delayed CP in his pelvic limbs with the left leg worse than the right. He had normal tone and reflexes. He had equal muscle mass in both pelvic limbs. Perineal reflex and anal tone were normal. He had kyphosis associated with his thoracolumbar and cervicothoracic spine with associated hair coat changes. Palpation of his thoracic spine over the area of kyphosis revealed an abnormal curvature toward the left (palpable from approximately T3-T11). His abnormal spine made it difficult to palpate vertebral spaces with precision; therefore, I used rib spaces to approximate. There was decreased range of motion (ROM) on shoulder extension bilaterally and with neck movement in all directions (left worse than right). He walked with a stiff neck that was held slightly toward the right. He used his entire body to turn or look in different directions instead of moving his neck. Gait evaluation revealed a short stride in the forelimbs and abduction and circumduction of his pelvic limbs. While he had use of his pelvic limbs, he relied on his forelimbs to rise from a lying to a standing position. Myofascial exam revealed restriction and taut bands along his entire cervical and upper thoracic spine. He had tension and restriction in multiple muscles in the region including the semispinalis capitis, trapezius, splenius capitis, longissimus capitis, rhomboids, latissimus dorsi, erector spinae, omotransversarius, sternocephalicus, and brachiocephalicus. While his owner did not feel Francis was painful he did appear to resent gentle extension of his shoulder on the left, gentle extension of his carpus on the left, and on hip abduction bilaterally. His reactions were subtle but obvious. Palpation along his spine did not elicit obvious pain.
Problem List and Differentials
Problem List:
Bilateral carpal valgus (worse on left), kyphosis of cervicothoracic and lumbar spine, pelvic limb paresis and ataxia, myofascial restriction in the cervical and thoracic spine, mild bilateral hip pain, brachycephalic airway syndrome, decreased range of motion of shoulders, mild left carpal pain on flexion
Differentials:
1: Kyphosis of the cervicothoracic and lumbar spine: Vascular: thrombosis/infarct, ischemic injury, Infectious/Inflammatory: diskospondylitis, osteomyelitis, Neoplastic: osteosarcoma, fibrosarcoma, chondrosarcoma, other soft tissue or metastatic lesion, Degenerative: osteoarthritis, degenerative disc, spondylosis, Iatrogenic/Intoxication: neurotoxins, Congenital: hemivertebrae, block vertebrae, butterfly vertebrae, scoliosis, spina bifida, Autoimmune: immune mediated arthritis, rheumatoid arthritis, immune mediated myositis or neuritis, Traumatic: fracture, traumatic disc, trauma from fall or rough play, Endocrine/Metabolic: calcium/vitamin D deficiency, Myofascial: myofascial tissue restriction, nerve entrapment, referred pain to myofascial (somatic or visceral).
2: Pelvic limb paresis: Vascular: Fibrocartilaginous embolism (FCE), other thromboembolism/infarct, ischemic injury, Infectious/Inflammatory: diskospondylitis, distemper myelitis, bacterial/fungal/protozoal myelitis, Neoplastic: primary skeletal, metastatic, lymphoreticular neoplasm (osteosarcoma, fibrosarcoma, chondrosarcoma, lymphosarcoma, plasma cell myeloma), Degenerative: degenerative intervertebral disc disease (IVDD), spondylosis, degenerative myelopathy, demyelinating diseases, Iatrogenic/Intoxication: neurotoxin, iatrogenic trauma from inappropriate injection, Congenital: hemivertebrae, block vertebrae, butterfly vertebrae, scoliosis, spina bifida, Autoimmune: immune mediated neuropathy, Traumatic: fractures, luxation, contusion, Endocrine/Metabolic: endocrine neuropathy, hypothyroidism, diabetes mellitus, Myofascial: myofascial tissue restriction, nerve entrapment.
Putative Diagnosis
Francis had a T3-L3 myelopathy causing upper motor neuron (UMN) paraparesis and ataxia. Spinal radiographs revealed numerous malformed vertebrae and an abnormal curvature of the spinal column. An MRI diagnosed severe scoliosis and kyphosis associated with vertebral malformations from T5-T10 causing moderate to severe left sided spinal cord compression. The kyphosis and myofascial restrictions in the area are likely secondary to the spinal abnormalities as well as the constant off-loading from the paraparesis. The kyphosis in the lumbar region is likely due to abnormal spinal conformation, off-loading, and myofascial restriction. The carpal valgus is a congenital malformation that is common in chondrodysplastic breeds. It is likely that it became more severe on the left side due to the off-loading and unequal distribution of weight during ambulation due to the paraparesis. The mild hip pain may be due to hip dysplasia that has not yet been diagnosed, osteoarthritis, or referred from the spinal cord. The decreased range of motion in the shoulders is likely secondary to myofascial restriction. To further characterize the clinical signs in the hips, shoulders, and carpi, additional radiographs would be necessary.
Pre-treament 1 Pre-treament Pre-treatment 2 Pre-treatment 3 Slow motion prior to tx
Medical Decision Making
My approach to treatment was based on both the goals of the owner and on my physical exam findings. The goal of the owner was to improve and maintain mobility, reduce/relieve any pain, allow for better movement with the pelvic limbs, and to try to get him off of his medication (steroid). I knew that it would not be possible to change his congenital spinal malformations; however, I wanted to address his myofascial restriction which would allow him to have better mobility and put less stress on his other joints secondary to unequal weight bearing. Neuromodulation of his pelvic limbs would allow him to walk with less ataxia and reduce some of the hip pain I noted. It would also take some of the pressure off of the thoracic limbs when walking and moving. Since he had never had acupuncture I made sure to go slow and use smaller needles initially. I used calming points at each visit. Because of his airway, I had to choose points that would give me the most benefit. He did not allow for all of the points I wanted to use as he did not like to lay on his side and became easily stressed. When he was stressed (even minimally) he developed upper airway signs. I used points that were easily accessible, led to minimal stress, and that could neuromodulate multiple areas at the same time.

Treatment-Medical Acupuncture and Related Techniques
11/6/2019-Initial consultation, exam and massage. During out first meeting, I discussed history and treatment goals, acupuncture and how it may benefit Francis, and I performed a through exam (general, neurological, orthopedic, and myofascial). We made a plan and scheduled future treatments. I ended our meeting by performing a massage using compression, effleurage, and petrissage. This helped Francis become comfortable with me and understand I was not going to hurt him. He was very receptive to the massage.
11/12/2019-First acupuncture treatment. Since Francis had never gotten acupuncture I used small, coated needles (Seirin 0.16x30mm) and selected calming points first. I used GV 14 (cervicothoracic spinal nerve point) as a local neck point to address cervicothoracic myofascial restriction as well as an autonomic point to neuromodulate parasympathetic tone and cause relaxation. Next I used Bai Hui (mid-caudal lumbar spinal nerve point) as an autonomic point to help with relaxation, a local point to address the lumbar kyphosis and myofascial restriction and to help neuromodulate the pelvic limbs (attempting to modulate the area of the spinal cord where the sciatic nerve emerges). Francis tolerated the needles. I waited approximately five minutes while Francis relaxed and ate baby food and then added additional points. I chose additional BL line points in the areas that I felt the most restriction (as central and local points). I wanted to address areas above and below the area of his spinal cord compression. I used BL 14, BL 17, BL 19, and BL 21. These addressed different spinal nerves (cranial thoracic, mid-thoracic, and thoracolumbar). Needles were left in place for thirty minutes before being removed. I finished our session with a massage that included his entire back, neck, chest and limbs. He was very relaxed and fell asleep while I was talking to his owner. His owner reported that he slept well that night and seemed more energetic in the morning. Overall, his owner was happy with the treatment.
11/20/2019: Francis came in willingly for his second acupuncture treatment. Before placing needles I did a myofascial exam. Compared to our first visit his cervical and cranial thoracic myofascial was much less restricted. It was a notable difference. His head was held less toward the right side than it had previously. His pelvic limb ataxia and carpal valgus was unchanged. My plan was to use bigger needles since he seemed to tolerate the smaller needles. I used a combination of Seirin 0.20x30mm (most areas), Seirin 0.14x15mm (for more sensitive areas), and Carbo 0.2x25mm (only one area as he was sensitive to these-BL20). I first used calming points (GV14, Bai Hui, and GV20-all with Seirin 0.20x30mm needles). The addition of GV 20 this week added to his relaxation. GV 20 was used for autonomic neuromodulation (via trigeminal and cranial cervical spinal nerves and crosstalk with the vagal nerve). Needles were left in place for five minutes before placing others. I placed needles based on myofascial palpation and on what Francis would allow. I used BL 10 to address local myofascial restriction (cranial cervical spinal nerves). He was sensitive to needles in this area and they were removed after a few minutes. I used BL11, BL13, 20 (for cervicothoracic, cranial thoracic and caudal thoracic spinal nerve stimulation). I used Seirin 0.2x30mm in all but BL20 where I tried Carbo 0.2x25mm (he was more sensitive to this needle). He did not allow for any points on the forelimbs or ventral neck so I wanted to address areas of the spinal cord where the nerves of the brachial plexus arise (C6-T2) in hopes of neuromodulating the nerves that innervate the forelimb and carpus. When I realized he was comfortable and relaxed I added hip points (GB29, GB30, BL 54) to address local pain and to neuromodulate the sciatic nerve. I used Seirin 0.14x15mm because he was sensitive with the larger needles. I added KI1 as a distal peripheral point to address the tibial nerve (Seirin 0.14x15mm).




Leaving after 2nd treatment (able to turn neck better)
11/26/2019: Francis ran into our exam room when he arrived for his third treatment. He appeared to be stronger than he had been when I did my initial exam. The owner reported similar findings at home. While his rear limbs were still ataxic, he seemed to replace them a little more quickly. The areas of restriction in his neck and movement in his neck were similar to the week before but improved from the initial exam. He appeared more comfortable with hip extension. I started with autonomic points for relaxation: GV20, GV 14, and Bai Hui (needles used this week were Seirin 0.20x30mm unless otherwise noted). These also acted as local points (mentioned in more detail in my first treatment). After a few minutes, I added points along the BL channel as both central and local points (BL 10, BL 13, BL 17, BL 20, BL 25, and BL 28). While he was still sensitive with BL 10 (I used Seirin 0.14X15mm), he allowed me to place the needles and kept them for the entire treatment. This was an important point for me because it was in an area of extreme myofascial restriction. I added peripheral points based on his exam and what he allowed. I used GB 21 for forelimb neuromodulation. He did not allow many other forelimb or ventral neck points. I was able to place a few Baxie points in the left to neuromodulate the carpus (Seirin 0.14x15mm). I used Bafeng points in both rear feet to provide neuromodulation for his pelvic limb paresis. He also allowed needles at ST 34 and 36 for femoral and fibular nerve stimulation. Needles were left in for thirty minutes with a few falling out before. The treatment ended with ten minutes of massage and passive ROM. The massage seemed to be his favorite part of treatment.

Video (2) copy Video (2) Video_1 (2) Video_2 (1)
Outcomes and Discussion
Francis had improvement in his myofascial restriction, pain, and overall mobility over the four weeks of treatment, as evidenced by my myofascial palpation as well as reports by the owner. He came in willingly showing his comfort with me and the treatments he was receiving. Knowing that I would be unable to fix his congenital issues, my goals were to reduce some of the myofascial restriction and pain caused by off-loading and unequal weight distribution during movement. One of the best things that we observed was that he wagged his tail. This was something that the owner had not seen before.
Chondrodysplastic breeds, like the English Bulldog, are predisposed to angular limb deformities and intervertebral disc disease. Selectively bred for a screw tail (hemivertebrae) predisposes them to spinal malformations that can include hemivertebrae and butterfly vertebrae. Hemivertebrae can cause kyphosis, scoliosis, and lordosis which can, in some animals, cause compression of the spinal cord. Signs associated with the compression usually stabilize once the vertebral growth plates fuse. The paraparesis that Francis developed caused him to unequally carry a great deal of weight with his trunk and forelimbs. His abnormal spine that is now fixed in place also adds to his myofascial restriction in the cervical and thoracic region.
I learned a great deal from this case. It was the first case I did after my intensives. It reinforced that the body does not work in isolation but is rather like one organ. A problem in just one area has great influence in all of the others. I learned how to be slow, gentle and never forceful. While I had a great, long list of points I thought would benefit Francis, I had to modify and use what he allowed. I learned how to choose points that affected nerves leaving the spinal cord at certain areas, thus allowing me to neuromodulate other nerves that arose from the same area. This was important when I wanted to use a point Francis would not allow. I could neuromodulate from a different point that he would allow. I learned how beneficial massage can be and that patients respond favorably to it. I look forward to continuing my treatment of Francis as well as new cases that come my way. When I see appointments in general practice now, I am always thinking of a way acupuncture would benefit the patient (it is almost every patient I see now).
References
1. Dewey CW, Davies E, Bouma JL. Kyphosis and kyphoscoliosis associated with congenital malformations of the thoracic vertebral bodies in dogs. Vet Clinics North American Small Animal Practice 2016; 46:295–306.
2. English Bulldog – Hemivertebrae
http://www.ufaw.org.uk/dogs/english-bulldog-hemivertebrae#clinical
3. Evans, H. and deLahunta, A. (2000) Guide To The Dissection Of The Dog-5th Edition.
4. Jeffery N, Smith P and Talbot C (2007). Imaging findings and surgical treatment of hemivertebrae in three dogs. Journal of the American Veterinary Medical Association 230: 532-536.
5. Johnson, K and Watson, A.D.J. (2000) Skeletal Diseases. In Ettinger S and Feldman, E (Eds) Textbook of veterinary internal medicine. 5th Ed. Philadelphia: WB Saunders Company.
6. Oliver, J,E. Jr., Lorenz, M.D., and Korgegay, J.N. (1997) Handbook of Veterinary Neurology –3rd Edition.
7. Robinson, N.G. (2017) CuraCore Medical Acupuncture for Veterinarians–Canine Point Mini Manual
8. Wyatt S., Goncalves R., Gutierrez-Quintana, R, and De Decker, S.
9. Outcomes of nonsurgical treatment for congenital thoracic vertebral body malformations in dogs: 13 cases (2009–2016) Journal of the American Veterinary Medical Association 2018 253:6, 768-773.