Written by a CuraCore Veterinary Medical Acupuncture course graduate. Signed release obtained from client/author. 10S2019011
ABSTRACT
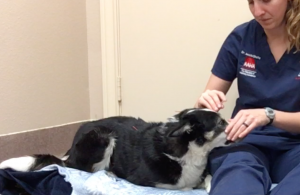
MsB, a 5-year-old intact female border collie used for competitive field trials, presented for consultation and acupuncture treatments to maintain performance as a canine athlete. Behavioral concerns mentioned by the owner included anxiety and hyperactivity. Myofascial restriction and taut muscle bands were noted in the thoracic limbs and neck, as well as muscle atrophy of the cleiodobrachialis and superficial pectoral muscles. The frequency of treatments was increased following an acute injury leading to a left front lameness at a field trial event. Acupuncture treatments focused on stimulating the atrophied muscles, releasing trigger points, and treating suspected headaches resulting in a return to a normal gait, decreased myofascial restriction, and improved behavior.
HISTORY OF PRESENT ILLNESS AND CHIEF COMPLAINTS
Signalment: 5-year-old intact female border collie
Chief Complaints: Initial consult had “no concerns”, but behavioral anxiety and hyperactivity issues were noted (front left lameness developed after initial consult and acupuncture treatment).
Lifestyle Factors: Used for competitive field trials (2 to 3-day long competitions with multiple runs and an assistant role during other dogs’ trial runs). Maintenance exercise plan includes working on a large property with livestock, running three miles 2 to 3 times a week.
History of Present Illness:Patient has been performing in competitive field trials for 3 years. Handler has difficulty matching the energy level of dog while still remaining calm (essential for competition). Anxiety was previously diagnosed in medical record on 10/18/18. Patient’s gait was normal during assessment on 11/20/19. Competed on 11/29/19 through 12/1/19 (3 primary runs with 2 assist runs) and developed a left front lameness.
Past Medical History:
7/19/19: Last bloodwork (no abnormalities)
7/23/18: dystocia with one puppy (born alive) and mummified fetus
6/6/18: dermatitis and otitis externa secondary to allergies, managed with cytopoint injections
1/3/18: Acute right rear lameness resolved on its own, treated once with laser and Adequan injections (continued as monthly injections, last injection in October)
8/3/17: Grade I-II/VI heart murmur auscultated, unremarkable radiographs, no additional diagnostics or treatments instituted
PHYSICAL EXAMINATION AND CLINICAL ASSESSMENT
Vital Signs: Heart rate: 120 bpm; Respiratory rate: 28 bpm; Temperature not taken
Standard Physical Examination:
• Weight: 32 lbs
• General Appearance: bright, alert, responsive, Fear Anxiety Stress score 3/5
• Integument: Hair line at Bl15, hair lines rostral-lateral from GV20
• Oral Exam: mild calculus on premolars, staining on canines
• Ophthalmic: normal clear cornea and anterior chamber OU
• Otic: clear AU with no discharge
• Auscultation: no murmur, sinus arrythmia; quiet, soft bronchovesicular sounds
• Abdomen: soft abdomen, body condition score 3/5
• Lymph Nodes: normal soft and symmetrical
• Skeletal: hesitant to bear weight fully on left front intermittently during proprioceptive testing, range of motion of front and hind limbs normal, range of motion of neck normal
• Urogenital: normal with no discharge from vulva
Neurologic Assessment:
Mentation: normal; Posture and gait: normal; Cranial nerves: normal; Proprioceptive placing: normal; Biceps and patellar reflexes: normal
Myofascial Evaluation:
Multifocal taut muscle bands and fascial restrictions in the cranial aspect of the cleidocephalicus, sternocephalicus, and omotranversarius muscles with the bands on the right side larger than the left. Muscle atrophy (mild) on left front cleiodobrachialis and superficial pectoral muscles. Fascial restriction over the caudal aspect of the skull at GV20 and radiating laterally. Taut muscle bands bilaterally at BL15
PROBLEM LIST
1. Muscle atrophy on left front (later developed lameness)
2. Hyperactivity, high intensity, anxiety
3. Taut muscle bands and fascial restriction in the neck and back
4. Fascial restriction over the head
DIFFERENTIAL DIAGNOSES FOR TOP TWO PROBLEMS
1. Left front muscle atrophy
V- cardiomyopathy, endocarditis, embolism; I- myositis, local vasculitis, infectious arthritis, osteomyelitis, sarcocystis; N- lymphosarcoma, paraneoplastic syndrome (cachexia), brachial plexus nerve tumor; D- shoulder/elbow/carpal arthritis, shoulder instability, myopathy, neuropathic pain; I- thyroid hormone ingestion; C- cervical vertebral misarticulation, congenital myopathy, luxation of scapulohumeral joint; A- immune-mediated arthritis; T- brachial plexus injury, traumatic fracture, laceration/ruptured tendon, exercise induced sprain/strain; E- diabetes, hyperadrenocorticism, hyperthyroidism, vitamin e deficiency, pathologic fractures; M- muscle soreness/contracture, clavicular intersection contracture, compression of cervical spinal nerves
2. Hyperactivity, high intensity, anxiety
V- cardiomyopathy, congestive heart failure; I- otitis, masticatory muscle myositis, canine distemper virus; N- intracranial/brainstem tumor, paraneoplastic syndrome (hypoglycemia); D- myopathy, neuropathic pain, osteoarthritis; I- pseudoephedrines ingestion, amphetamine ingestion, thyroid hormone ingestion, lead toxicity, caffeine ingestion, cannabis ingestion, fears/phobias; C- skull/cervical malformation, vertebral column dysplasia; A- immune-mediated arthritis, allergic reaction; T- skull/nasal trauma, emotional trauma; E- hyperadrenocorticism, hyperthyroidism, thiamine deficiency, eclampsia, pregnancy hypocalcemia; M- muscle soreness, compression of cranial/spinal nerves
DEFINITIVE DIAGNOSES FOR TOP TWO PROBLEMS
1. Left front muscle atrophy: muscle soreness and contracture
Based on the patient’s history as an athlete and the development of a left front lameness following a competition, the top differential for the muscle atrophy was muscle contracture and soreness following chronic high intensity use. Other top differentials include changes to the fascia and musculoskeletal system or a historic injury with secondary muscle atrophy due to an adaptive change in the patient’s muscle use. These differentials were less likely at the initial diagnosis because the patient’s gait was normal and there was no history of any injury. A larger disease process is unlikely since the remainder of the physical examination was normal.
2. Hyperactivity, high intensity, anxiety: fascial compression of the facial nerve
The behavior concerns noted by the owner coupled with the myofascial changes are similar to the changes noted in some people with migraine headaches. I attributed the behavioral concerns to compression of a nerve secondary to compensation by the neck’s myofascia, however chronic pain could have a similar affect. Likewise, behavior changes could have occurred secondary to a traumatic emotional event. Behavioral concerns may develop secondary to a historic problem (cardiomyopathy, otitis, allergies) or something not currently diagnosed on physical exam. The intoxication differentials do not fit with the patient’s history but cannot be ruled out.
MEDICAL DECISION MAKING
At the time of the initial consult, the owner and I discussed that maintenance or improvement of performance was their main goal. Based off of physical examination, we decided that the front left leg would need extra attention since it had signs of muscle atrophy. The additional changes to the muscles of the neck and back could be secondary to the left front limb’s muscle atrophy, so we would provide supportive dry needling and massage to those areas. The changes appeared chronic since they were widespread with no inciting cause in the history; despite the muscle atrophy, taut bands, and fascial restriction there was no change to the patient’s gait. A conservative once a month treatment plan was originally agreed upon to match the owner’s performance goals. A Medical Acupuncture and Integrative Neuromodulation (MAIN) approach was developed to address the changes to the front left leg, but it also addressed myofascial restriction over the head, neck, and back. The behavior concerns were a concurrent issue that I thought may respond positively to the acupuncture treatments. As the patient’s comfort with treatment increased, we were able to add in additional points to address potential causes of the behavioral concerns. Photobiomodulation and electrostimulation may have been beneficial modalities for this patient, but were unavailable.


MEDICAL ACUPUNCTURE AND RELATED TECHNIQUES USED
Dry needling and manual therapy were selected as treatment modalities based off of the availability of equipment and the patient’s compliance with these treatments. After the initial treatment session, the initial once a month treatment plan was modified to once a week due to an acute episode of lameness on the left front leg.
The initial treatment session involved 10 minutes of general effleurage to identify myofascial changes followed by 10 minutes of petrissage of the cleidocephalicus, sternocephalicus, omotranversarius, longissimus, and superficial pectoral muscles to stimulate the myofascia and release tension in peripheral trigger points. Each subsequent session contained at least 10 minutes of petrissage to facilitate the release of muscle tension. The owner was able to use effleurage at home between sessions over the patient’s myofascial restriction points, especially the cranial neck region.
The initial acupuncture session consisted of 6 Seirin J type 0.12 x 30mm needles. Central neuromodulation was provided by GV 14 and was used in every subsequent treatment session. GV 20 also served as a central neuromodulation point at every session but had the added benefits of decreasing myofascial restriction and increasing autonomic regulation. Additional autonomic regulation points used to decrease inflammation came from dry needling of ST36 and LI11. The stimulation of both of these points was well-tolerated at the initial visit but had to be modified at subsequent visits due to increased patient sensitivity. Myofascial restriction was addressed with GV14 and BL10 at all treatments. Peripheral stimulation was provided by petrissage of the superficial pectoral muscles. Due to the patient’s moderate level of reactivity over the superficial pectoral muscles, acupressure was used at LU1 rather than dry needling. The patient tolerated this session well, and a plan to increase needle size was instigated.
Seirin J type 0.16 x 30mm needles were used at all subsequent treatment sessions except at GV20 and Yintang at treatment session #2 and #3 which required 0.12 gauge needles. Additional myofascial restriction was noted caudal to the taut bands identified at BL15. The patient was too sensitive for dry needling in this band, so central stimulation was provided with dry needling of BL14 and BL10. The hairline at GV20 seemed more noticeable with increased myofascial restriction of the muscles of the caudal head and cranial neck. Yintang was added to the treatment protocol for additional relaxation and to treat suspected headaches. While the central and autonomic points remained consistent, the peripheral and myofascial points were expanded. Peripheral points that were added included cervical spinal nerve points, GB14, and SI11. Myofascial trigger points that were treated included BL13, BL15, LU1, and a point along the hairline of the caudal head that was 1 cun lateral to GV20.
Gait 12_18_19 lateral Gait 12_18_19 towards and away
OUTCOMES AND DISCUSSION
The owner’s initial goal for acupuncture treatments was to maintain MsB’s performance as an athlete. However, after our initial treatment session and discussion about the various myofascial restriction patterns and muscle atrophy, the owner was considering a more frequent treatment plan to help avoid injury. Unfortunately, the patient suffered an injury while working which promoted this more aggressive treatment plan.
Interestingly, the patient developed a lameness after the initial consultation following a field trial competition. The owner attributed this lameness episode to an acute injury such as a strain or sprain despite not seeing an inciting event. If the initial consult had occurred following this injury, then it would have been easy to attribute the muscle atrophy of the left cleiodobrachialis and superficial pectoral muscles to the injury rather than the other way around.. Since the muscle atrophy and taut muscle bands were predisposing factors to the injury, I focused my acupuncture treatments to the nerves of the neck, shoulders, and back. Although some trigger points were released, there would still be at least two or three taut muscle bands along the Bladder meridian following treatments. After each acupuncture session, the owner and I noted improvement to the left front lameness. At the end of treatment session number four, more symmetrical muscling over the pectoral muscles and neck muscles was noted.
At the initial acupuncture session, MsB was very noise reactive and hesitant to stay in a “down stay” for more than 5 minutes. She was graded as a Fear, Anxiety, Stress (FAS) score of 3/5 based on body posture, avoidance behaviors, and reactivity to stimulus. At treatment session #4, MsB was graded as a FAS score of 1/5 with a more relaxed body position and decreased reactivity to stimulus. She even started taking treats following her sessions indicating an FAS score of 0/5. The most surprising outcome was the decrease in anxiety and hyperactivity noted by the owner for multiple days following an acupuncture session. Despite being on a reduced exercise plan, MsB appeared calmer at home and more responsive to commands. Although the patient did not show episodes of vocalization or fear behaviors seen with other case reports of suspected migraines in dogs, it is interesting to note the change in demeanor and improvement to the myofascial restriction patterns following acupuncture treatments.
REFERENCES
• Desai, M.J., Saini V., & Saini S. (2013), Myofascial Pain Syndrome: A Treatment Review. Pain Ther, 2: 21-36. doi:10.1007/s40122-013-0006-y.
• Fu, L.M., Li, J.T., & Wu W.S. (2009), Randomized controlled trials of acupuncture for neck pain: systematic review and meta-analysis. J Altern Complement Med, 15(2): 133-145. doi:10.1089/acm.2008.0135.
• Kong, L.J., et al. (2013), Massage therapy for neck and shoulder pain: a systematic review and meta-analysis. Evid Based Complement Alternat Med, Feb. doi:10.1155/2013/613279.
• Plessas, I., Volk, H., & Kenny, P. (2013), Migraine‐like Episodic Pain Behavior in a Dog: Can Dogs Suffer from Migraines?. J Vet Intern Med, 27: 1034-1040. doi:10.1111/jvim/12167.